 Humans obtain vitamin D from two sources. Firstly, humans are able to synthesise vitamin D in their skin. This cutaneous reaction is catalysed by ultraviolet light and results in the production of vitamin D3, also called cholecalciferol. Humans can also ingest vitamin D from their diet. Vitamin D is present in the diet in two main forms. Animals produce cholecalciferol just like humans, and when we ingest animal products we ingest vitamin D3. Microorganisms including bacteria however produce ergocalciferol (vitamin D2) and so the ‘plant’ form of vitamin D differs chemically. Essentially both sources of vitamin D enter a common pool of vitamin D and both can be utilised by human metabolic processes, although vitamin D2 shows slightly lower bioavailability. In the absence of sunlight, humans must obtain their vitamin D from the diet. However, calculating equivalences between sunlight obtained vitamin D and dietary obtained vitamin D is difficult because of the different ways the vitamin can be transported.
Humans obtain vitamin D from two sources. Firstly, humans are able to synthesise vitamin D in their skin. This cutaneous reaction is catalysed by ultraviolet light and results in the production of vitamin D3, also called cholecalciferol. Humans can also ingest vitamin D from their diet. Vitamin D is present in the diet in two main forms. Animals produce cholecalciferol just like humans, and when we ingest animal products we ingest vitamin D3. Microorganisms including bacteria however produce ergocalciferol (vitamin D2) and so the ‘plant’ form of vitamin D differs chemically. Essentially both sources of vitamin D enter a common pool of vitamin D and both can be utilised by human metabolic processes, although vitamin D2 shows slightly lower bioavailability. In the absence of sunlight, humans must obtain their vitamin D from the diet. However, calculating equivalences between sunlight obtained vitamin D and dietary obtained vitamin D is difficult because of the different ways the vitamin can be transported.
One of the main differences between the vitamin D synthesised in the skin and the vitamin D obtained in the diet is the initial transport route for the vitamin. For vitamin D to be used metabolically it must first be transported to the liver in order to undergo a process called hydroxylation. Hydroxylation is essentially adding an -OH or hydroxyl group somewhere on the molecule. This alters the chemistry of the molecule and creates 25-hydroxyvitamin D (also called 25-hydroxycholecalciferol) which is the metabolite measured to assess vitamin D status. Vitamin D synthesised in the skin following exposure to ultraviolet B radiation is transported almost exclusively from the skin to the liver by a protein called the vitamin D binding protein (DBP). This protein is required because vitamin D is a lipid and will not dissolve in the blood. Combining the vitamin D with a protein improves the solubility of the vitamin D and allows it to be transported in the blood to the liver, where it is then hydroxylated.
Dietary sources of vitamin D are cholecalciferol (vitamin D3) or ergocalciferol (vitamin D2). Studies suggest that vitamin D3 has superior bioavailability. However, dietary sources oof the vitamin may be less efficiently used than cutaneous sources.
In contrast, the vitamin D (as cholecalciferol and ergocalciferol) consumed in the diet (eggs, fish and liver are the main sources) is absorbed into the gut cells and packaged into a protein carrier called a chylomicron. This process of package into chylomicrons is essentially the same process that is used to absorb other dietary lipids from the gut. Vitamin D is therefore absorbed from the gut along with other lipids in the diet such as triglycerides and cholesterol. As with the vitamin D binding protein, the chylomicron is necessary because lipids cannot dissolve in the blood and therefore a protein must be used to transport them. The chylomicrons formed in the enterocytes, along with their vitamin D content, pass into the lymphatic system and then to the blood. Some of the lipids in the chylomicrons are passed to peripheral tissue such as fat cells (adipocytes). The remnants of the chylomicron and its content then pass to the liver where the chylomicron is broken down, and the vitamin D is removed and hydroxylated.
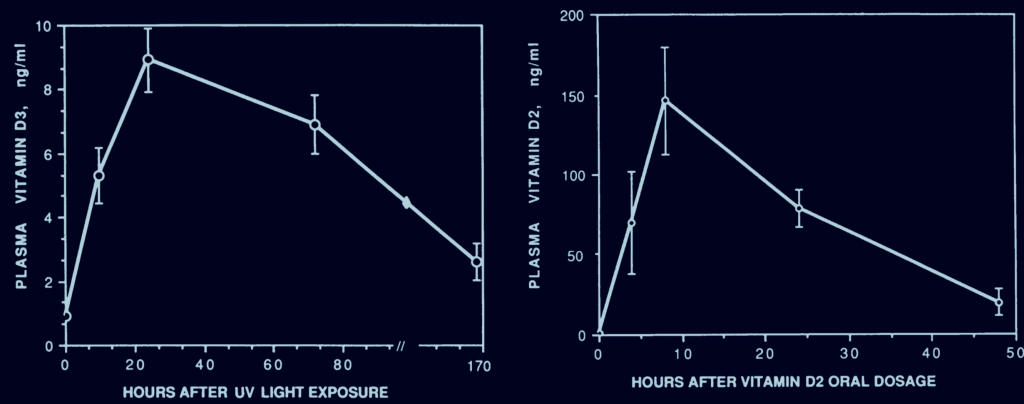
The relatively prolonged increase in the blood levels of cutaneously produced vitamin D (left) is due to the slow release of the vitamin from the skin. However, this is not the only factor. Administration of vitamin D as an oily depot injection to the muscle results in a more rapid rise that the vitamin D produced naturally in the skin by the action of ultraviolet light. This is likely explained by the high affinity of the cutaneously produced vitamin D for the vitamin D binding protein. Depot injections of vitamin D likely use other carrier proteins and this may therefore cause a more rapid rise in blood levels and a more rapid transport and delivery to the liver, ultimately speeding up metabolism and inactivation of the vitamin to water soluble conjugates.
Therefore differences exist between the routes of vitamin D transport to the liver and this creates differences in the efficiencies of cutaneous and dietary sources of the vitamin. The cutaneously produced vitamin D diffuses slowly from the skin to the circulation and this creates a slow and prolonged increase in vitamin D levels. In contrast, the vitamin D absorbed in chylomicrons is more rapidly absorbed to the blood and this creates a more rapid and less prolonged rise in vitamin D levels. The subsequent levels of 25-hydroxyvitamin D reflect the increases in the parent compounds of vitamin D, and therefore cutaneous production of vitamin causes a slow and prolonged increase in 25-hydroxyvitamin D, compared to dietary sources. The hydroxylation of vitamin D metabolites by the liver can eventually inactive it, and as the cutaneous production of the vitamin slows the passage to the liver, the vitamin D produced in the skin prolongs the activity of the vitamin D for longer periods.
Eat Well, Stay Healthy, Protect Yourself
RdB
