Calcium is a major structural component of bone and deficiencies of calcium cause bone abnormalities. However, the interaction between calcium in the diet and bone health is controversial, and studies showing beneficial effects of calcium supplements on osteoporosis are inconsistent, and some reviewers have questioned the benefits of supplements in postmenopausal women. However, although controversial, some studies have shown positive effects for calcium supplements on some of the markers that signify bone loss. For example, in one study1, researchers gave 1 gram per day of calcium supplements to 14 postmenopausal osteoporotic women. After 8 days the fasting hydroxyproline to creatinine ratio, one measure of bone loss, had decreased significantly. In addition, plasma phosphate increased significantly due to decreased excretion by the kidney. Low plasma phosphate and increased excretion is a symptom of elevated parathyroid hormone, which can become elevated in an effort to raise low levels of plasma calcium (figure 1).
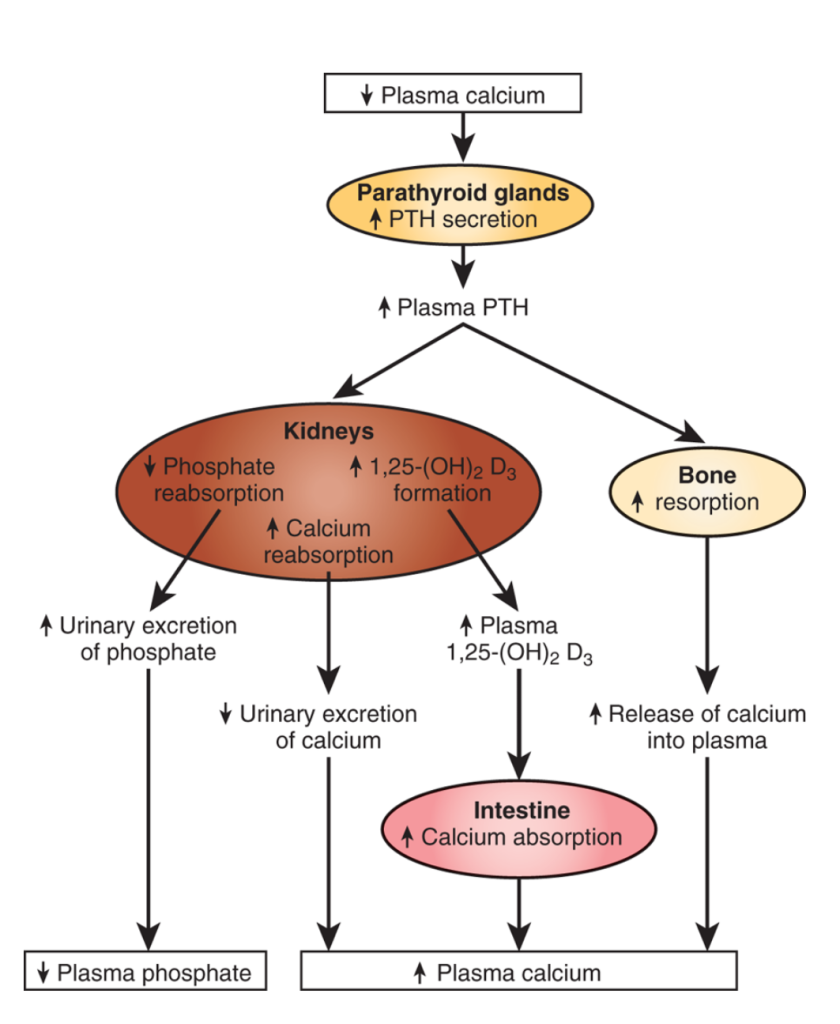
Figure 1. The relationship between phosphorus, calcium and parathyroid hormone. (Taken from Medical Physiology, Principles of Clinical Medicine by Rhoades and Bell).
So the calcium supplements in this study may have been effective at altering the calcium bone balance to one in which calcium bone loss was reduced. The results from this study are similar to many other studies that have looked at biomarkers of calcium loss. Calcium supplements improve markers of calcium loss from bone, at least in the short-term, and therefore there is some evidence they may be effective. The main controversy surrounding the use of calcium supplements is that when studies investigate their ability to reverse or prevent osteoporosis, there is no consistent improvement in the subject’s risk of the disease. This is an interesting point to discuss because it is a similar pattern seen with many other nutritional approaches. A single nutrient can affect markers of a particular disease or condition, but when the nutrient is given long-term, the risk does not change significantly. So why does this occur and what are the factors that can be considered to rectify the lack of efficacy in such circumstances?
The likely reason that calcium supplements are not a magic bullet that can reverse osteoporosis is because the disease is not caused by solely by a low intake of calcium. More recent evidence is starting to highlight the Western diet as a driver of Western lifestyle diseases such as osteoporosis. In this regard, it is not the lack of calcium in the diet that causes the bone disorder, although it is undoubtedly a contributory factor, but the diet as a whole. Yes the diet is low in calcium, but it is also too high in phosphorus, contains too much acid forming foods such as red meat, too few plant foods and many other imbalances. Addressing one of these factor while continuing adherence to a Western diet is therefore akin to restoring a classic car by changing only the spark plugs. Might it make a difference? Yes sure that is possible. However, only by addressing all the faulty components of the car will it run and drive like its designer intended. This pattern is seen a lot within nutritional research, and care should therefore be taken when interpreting such interactions.
RdB
