 Homocysteine levels can be modulated through nutritional changes. It was over 30 years ago that Kilmer McCully proposed that elevated plasma concentrations of homocysteine were responsible for the damage to the artery walls that can lead to atherosclerosis. His observations were based on a child dying of a genetic defect in homocysteine metabolism called homocystinuria. The high levels of homocysteine in this patient resulted in arterial lesions surprisingly similar to those seen in cardiovascular disease. In the intervening years since this discovery, homocysteine has been identified as an independent risk factor for vascular disease. You would have thought with such a great discovery that McCully would be a hailed a hero, and that doctors and health care professionals would be scrambling over themselves to inform the public about homocysteine and its role in disease. However, there has been a complete silence concerning homocysteine from nearly all mainstream health care professionals. The reason for this is, as always, to do with money and profit. However, if you are interested in preventing cardiovascular disease, bypassing the mainstream ‘experts’ and educating yourself on the biochemistry of homocysteine may be of considerable benefit.
Homocysteine levels can be modulated through nutritional changes. It was over 30 years ago that Kilmer McCully proposed that elevated plasma concentrations of homocysteine were responsible for the damage to the artery walls that can lead to atherosclerosis. His observations were based on a child dying of a genetic defect in homocysteine metabolism called homocystinuria. The high levels of homocysteine in this patient resulted in arterial lesions surprisingly similar to those seen in cardiovascular disease. In the intervening years since this discovery, homocysteine has been identified as an independent risk factor for vascular disease. You would have thought with such a great discovery that McCully would be a hailed a hero, and that doctors and health care professionals would be scrambling over themselves to inform the public about homocysteine and its role in disease. However, there has been a complete silence concerning homocysteine from nearly all mainstream health care professionals. The reason for this is, as always, to do with money and profit. However, if you are interested in preventing cardiovascular disease, bypassing the mainstream ‘experts’ and educating yourself on the biochemistry of homocysteine may be of considerable benefit.
Homocysteine is an amino acid that is produced in the body from the essential amino acid methionine that we derive from the protein in our diets. Methionine is converted in the body to S-adenosylmethionine (SAM) and then to homocysteine. Once the the homocysteine is formed it can have one of two fates. Firstly it can be converted back to methionine. This pathway requires the enzymes methionine synthase and a methyl group from tetrahydrofolate. Alternatively the homocysteine can be converted to another amino acid called cysteine. In this second pathway the enzyme needed is called cystathionine beta-synthase. Like most enzymes methionine synthase and cystathionine beta-synthase require co-factors to allow them to work. Cofactors are vitamins or minerals that bind to the enzyme and allow it to perform it function by altering the shape of the molecule. In the case of the enzymes required for homocysteine metabolism methionine synthase and cystathionine beta-synthase require the vitamins B12 and B6, respectively. Tetrahydrofolate is also requires folic acid for its structure.
If these enzymes fail to metabolise homocysteine, the amino acid starts to build up in the body and higher levels can be detected with a blood test. In order to understand the problems associated with high homocysteine levels it is a good idea to look at the metabolic disorders that can raise levels in the blood and the consequences of this. Afterall, this is how McCully first identified the link between homocysteine and vascular injury. Given an umbrella term of homocystinuria, high homocysteine levels can be caused by a raft of genetic defects in the enzymes that are involved in the metabolism of homocysteine. These can include cystathionine beta-synthase, methylenetetrahydrofolate reductase and the methionine synthase enzymes. The results of these defects is an inability to convert homocysteine to its metabolic products, which in turn result in elevations of homocysteine levels to over 100 umol/L. This figure is roughly ten times the normal levels. High levels of homocysteine have been shown to be able to damage arterial walls and cause vascular damage, probably by free radical action and inhibition of nitric oxide synthase.
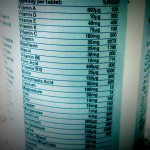
While metabolic defects in the enzymes themselves can cause a rise in homocysteine levels, it has also been shown that those without the defect but with a deficiency of the necessary enzyme cofactors, can also encounter raised homocysteine levels. For example, a paper published in the Journal of Nutrition in 1996 demonstrated that plasma concentrations of folate, vitamin B6 and B12 were inversely associated with homocysteine levels in human subjects1. In this study the researchers showed that not only did folic acid lower elevated homocysteine levels, it also reduced levels considered to be within the normal range (suggesting they are not normal). In another study in the Journal of Nutrition in 2000, consumption of a multivitamin supplement containing folate, B12 and B6, resulted in a reduction in homocysteine levels by 9.6 % in 56 days in healthy individuals2. These results suggest that not only does a deficiency of the B vitamins cause a rise in homocysteine levels. But in addition, that correction of that deficiency allows homocysteine levels to be reduced. The second study also provides further evidence for the efficacy of multivitamin supplements.
In addition to the B vitamins, supplementation with betaine has also been shown to be effective in the reduction of high plasma levels of homocysteine. For example, in a study published in the Journal of Nutrition in 2003, researchers reported that supplementation of 6 grams of betaine for 6 weeks was highly effective in lowering plasma homocysteine in subjects with moderately elevated homocysteine levels, although the betaine was not as effective as 800 micrograms of folate3. Betaine is effective at reducing homocysteine levels because it can cause the conversion of homocysteine to methionine via a different pathways than methionine synthase (the B12 route). Betaine is incorporated into the enzyme betaine homocysteine methyltransferase as a cofactor and this allows the metabolism of homocysteine to methionine through an alternative ‘salvage pathway’. Betaine is present in food but only in low levels and so to get it benefit on homocysteine supplementation is usually necessary. Quinoa, spinach, wheat-bran cereal and beets all contain betaine.
Although evidence shows that fruit and vegetables are good for the health, researchers are still unclear of the exact mechanisms of this potential benefit. Scientists have theorised that factors such as the fibre, antioxidants, or minerals may all account for the benefits seen to the health. However, it could well be that some of the beneficial effects of fruit and vegetables come from their reasonably high content of folate. A study published in the Journal of Nutrition in 2000 demonstrated that in test subject fed fruit and vegetables containing just 13.3 mg of folate, a reduction in homocysteine levels of 11 % was seen4. This is a relatively small amount of folate compared with the trials using vitamin supplements. The diets included a wide range of fruit and vegetables including french beans, red sweet peppers, onions, cucumber, tomatoes, carrots, apples, lettuce, cauliflower and mushrooms. In another study in the Journal of Nutrition in 2003, high intake of refined cereals was associated with low B vitamin and high homocysteine concentrations, whereas the consumption of fruit and milk was associated with low homocysteine concentrations5. Garlic may also be able to lower plasma homocysteine concentrations (here).
So why have mainstream medicine almost completely ignored the role of homocysteine in vascular disease? Well, expensive drugs are often touted as the solution to complex metabolic problems by the vested interests of big pharma. Unfortunately for them, there is a very simple treatment for high homocysteine levels that is also very cheap and readily available. Supplementary folate, B12 and B6 are able to moderate homocysteine blood levels and have been shown to be inversely associated with homocysteine intakes and blood levels. This is probably the reason that the pharmaceutical companies, mainstream medicine and the media have decided instead to concentrate all their marketing efforts on the role of cholesterol in heart disease. If you do not currently take a multivitamin with high levels of the B vitamins, this may be a great place to start in improving your vitamin and mineral status (here). In addition, it would seem prudent to try to avoid processed cereals and instead increase high folate containing fresh fruit and vegetable into your diet.
RdB
