The generally accepted biomarker for vitamin D status in humans is plasma 25-hydroxyvitamin D [25(OH)D]. Plasma levels of 25(OH)D can be maintained above the recommended 40 nmol/L through sunlight exposure or through dietary intake. Evidence suggests that modern lifestyle behaviours that result in limited sunlight exposure, as well as vitamin D restricted diets, are causing widespread chronic depletion of plasma 25(OH)D. This is particularly evident at high latitudes during winter months. Plasma 25(OH)D below 25 nmol/L gives rise to the traditional vitamin D deficiency disease of osteomalacia and rickets in adults and children, respectively. However, levels between 25 and 40 nmol/L are considered insufficient. Vitamin D insufficiency puts individuals at risk of chronic long-term ill-health through development of insulin resistance and immune suppression. These may ultimately develop into cardiovascular disease and cancer. Although in its infancy, recent research suggests that vitamin D insufficiency may also cause muscle weakness.
Vitamin D is metabolised to 25(OH)D in the liver and is then subsequently metabolised in the kidney by either 1α-hydroxylase or 24-hydroxylase (figure 1). The 24-hydroxylase enzyme converts 25(OH)D to 24,25(OH)2D which has a low biological activity and therefore inactivates vitamin D. Ergocalciferol (vitamin D2), the form of the vitamin derived from plants, is more easily deactivated in this way, when compared to the animal vitamin D3 form. In contrast, 1α-hydroxylase converts 25(OH)D to 1,25(OH)2D which is the substrate for the vitamin D receptor (VDR). Because serum 25(OH)D concentrations are around 1000 times higher than 1,25(OH)2D, plasma 25(OH)D acts as a store of vitamin D to maintain plasma levels of 1,25(OH)2D. The VDR is a nuclear receptor which all cells are though to possess, but classic textbook target organs include the intestine, bone and kidneys. Here 1,25(OH)2D acts to maintain plasma calcium concentrations.
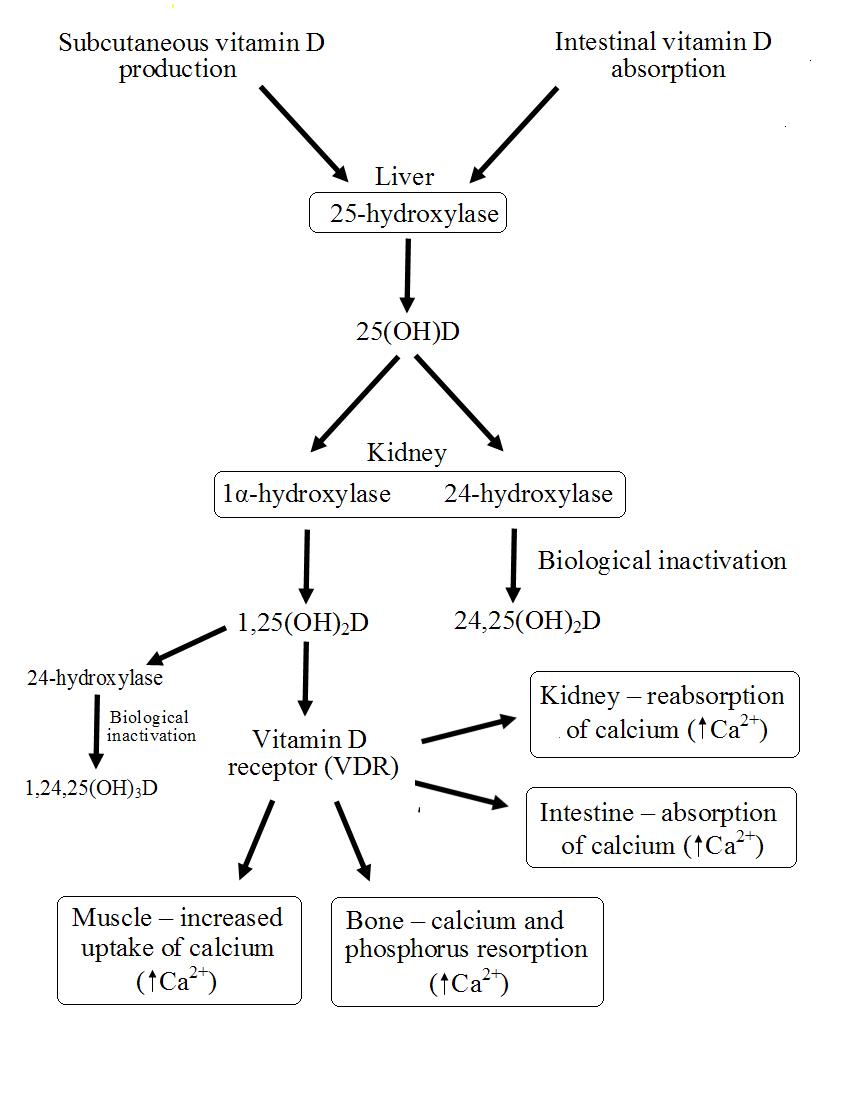 Figure 1. Metabolism of vitamin D in humans.
Figure 1. Metabolism of vitamin D in humans.
That 1,25(OH)2D may have an effect on muscle tissue is evidenced by the presence of the VDR in skeletal muscle. To date, interaction between 1,25(OH)2D and the VDR in skeletal muscle has been investigated mainly in animals models and is not fully understood. Observations of the rapid response of skeletal muscle to vitamin D supplementation has lead to suggestions of a membrane located receptor for vitamin D, which act through a second messenger network to cause cellular uptake of calcium. Studies investigating the role of vitamin D in muscle function in humans have largely been observational studies. A handful of studies have shown significant association between plasma 25(OH)D and muscle strength in elderly subjects. However, the cause and effect of this relationship is difficult to determine because a number of conditions that could cause similar weakness may stop individuals attaining adequate sun exposure.
Supplementation of elderly subjects with calcium and vitamin D for 8 weeks reduced body sway and resulted in a lower number of falls at a 1 year follow up when compared to calcium alone. This lead to the suggestion that vitamin D might predominately affect the load bearing postural muscles of the lower limb which are required for balance and walking. That vitamin D might affect muscle function is not surprising because in recent years many novel functions have been discovered for vitamin D, beyond its traditional role in calcium homeostasis. The discovery that many peripheral tissues, not considered traditional targets for vitamin, possess the VDR and the 1α-hydroxylase enzyme suggest that vitamin D is important in these tissues. Maintaining plasma 25(OH)D levels above the recommended 40 nmol/L requires intakes of around 14.5 µg/d (580 iu/d). In the absence of sunlight this is only possible with supplements.
RdB
